Torn labrum shoulder surgery can be very successful when used to treat symptomatic labral tears. Labral tears not causing symptoms do not require surgery. Therefore the key to treatment, and your shoulder specialist’s primary job, is to not only figure out if you have a labral tear, but also to try to determine if it is symptomatic. As you may recall from an earlier post, there are several types of labral tears: 1) Those that occur from significant trauma, such as a dislocation, 2) Those caused by repetitive microtrauma, as seen in throwing athletes, and 3) Those that are due to labral degeneration, as occur with increasing age. Degenerative labral tears may often be treated without surgery since they are frequently not symptomatic. However, labral tears caused by trauma, whether a single violent event or multiple smaller (micro-trauma) events, often require surgery.
Torn labrum shoulder surgery can be very successful when used to treat symptomatic labral tears. Labral tears not causing symptoms do not require surgery. Therefore the key to treatment, and your shoulder specialist’s primary job, is to not only figure out if you have a labral tear, but also to try to determine if it is symptomatic. As you may recall from an earlier post, there are several types of labral tears: 1) Those that occur from significant trauma, such as a dislocation, 2) Those caused by repetitive microtrauma, as seen in throwing athletes, and 3) Those that are due to labral degeneration, as occur with increasing age. Degenerative labral tears may often be treated without surgery since they are frequently not symptomatic. However, labral tears caused by trauma, whether a single violent event or multiple smaller (micro-trauma) events, often require surgery.
Torn Labrum Shoulder Surgery: Debridement
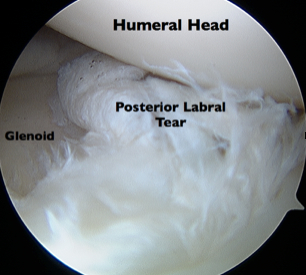
Some labral tears cause symptoms because the torn labral tissue irritates the adjacent lining of the joint (capsule). Others cause problems because the torn tissue gets caught in the joint as the shoulder moves. When this tissue is either of poor quality or the bulk of the labrum is attached to the glenoid (socket) and there is just a flap or small free piece of the intact labrum, the proper torn labrum shoulder surgery is usually a “debridement”.
During this type of surgery, the torn labral tissue is removed arthroscopically with some combination of a motorized shaver or scissor-like instruments. Although this reduces the overall amount of remaining labral tissue, the torn tissue was incapable of doing its job and so removing it only eliminates the symptoms. It does not adversely affect function or outcome (think of clipping a hangnail :-) ). Often since the bulk of the labrum in this location remains attached to the glenoid, the ligaments remain attached to the glenoid as well. Consequently, no instability of the shoulder occurs as a result of the debridement.
Furthermore, since the tissue is not repaired or reattached to the glenoid, there is no need to protect it after surgery. A sling is used briefly for comfort. Physical therapy can start immediately and no restrictions on activity, other than those due to your pain, are required. As a result, if you undergo a debridement as your torn labrum shoulder surgery, you can usually recover more quickly than had you had a labral “repair”.
Typically after this type of treatment, I expect improvement from the preoperative symptoms within 1-2 months and full recovery usually within about 3-6 months.
Torn Labrum Shoulder Surgery: Repair
In those situations in which good quality labral tissue is separated from the glenoid, the preferred torn labrum shoulder surgery is usually a labral repair.
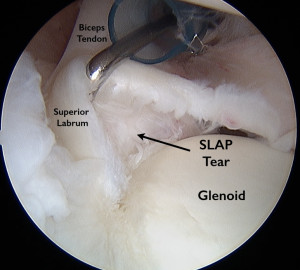
This is almost always the case in those who have sustained traumatic instability events (dislocations or subluxations). It may may also be needed, in overhead athletes (swimmers, throwers, volleyball players).
Labral repair surgery can be performed through larger incisions in an “open” manner or arthroscopically. Most labral repair surgery can be performed arthroscopically and so, except in some very unique cases in which there has been significant injury to the bone of the humerus (ball) and/or glenoid, I almost always perform labral repair surgery arthroscopically.
The major components of this surgery for me are:
- Outpatient (Go home the same day)
- Arthroscopic
- Address associated issues (Biceps tendinitis, subacromial bursitis, remove loose bodies, etc.)
- Remove any torn flaps of the labrum
- Mobilize the labrum if needed
- Promote bleeding at the glenoid attachment site
- Reattach the torn labrum to the glenoid using suture anchors
- Post op sling +\- ice sleeve
Watch the videos below to see arthroscopic labral repairs of tears at various locations on the glenoid.